Hyperhomocysteinaemia and low levels of vitamins B12 & D are associated with an increased risk of pregnancy loss (Bala et al, Lumme et al)
Multiple retrospective analyses of miscarriage associations with certain bio-markers have identified several nutrient deficiencies that are associated with an increased incidence of pregnancy loss. Some are also associated with higher levels of subfertility. By providing women with the lacking nutrients is it possible to reduce the risk of pregnancy loss? Instinctively it is logical to propose that appropriate supplementation combined with positive health and lifestyle changes can move the dial.
Hyperhomocysteinaemia is a term for the elevation of circulating homocysteine, an amino acid usually recycled by the one-carbon cycle. Raised levels indicate that the one-carbon cycle is operating sub-optimally, which raises the chances of cellular oxidative stress that can negatively affect egg and sperm generation and maturation and may also impede normal foetal development. Vitamin B12 is essential for normal homocysteine metabolism as it helps recycle it into an active intracellular agent in readiness to neutralise oxidative attack.
Vitamin D deficiency has been associated with an increased risk of abnormal pregnancy implantation leading to obstetric complications such as pre-eclampsia and fetal growth restriction. (Chu et al) Vitamin D (also referred to as 25(OH)D) regulates the production of sex hormones that can influence fertility in women and men. It is also suggested that it plays an immunomodulatory role and contributes to embryonic implantation, placentation and pregnancy success. Additionally, levels of the ovarian reserve marker, anti-Mullerian hormone (AMH), are positively correlated with 25(OH)D.
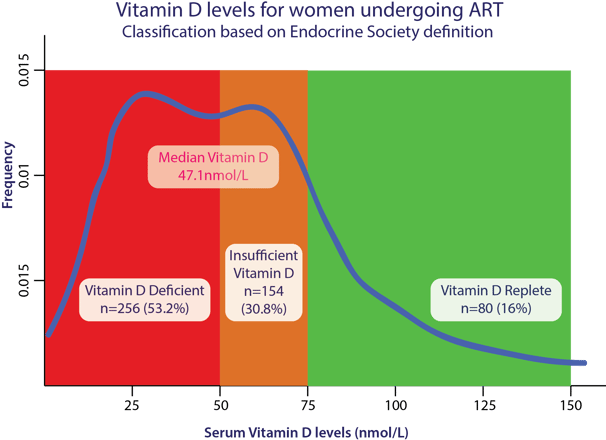
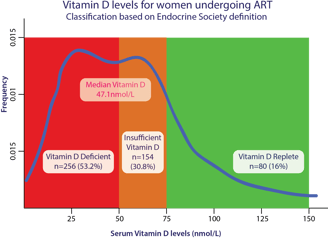
53.2% of women undergoing fertility treatment are vitamin D deficient
Researchers' Conclusion
"Vitamin D deficiency may be a treatable factor that can potentially improve the chances of ART success. Vitamin D serum testing is relatively cheap and widely available. Furthermore, treatment of deficiency or insufficiency with subsequent maintenance therapy is not costly and could also reduce the risk of obstetric complications such as gestational diabetes, preeclampsia, and fetal growth restriction." (Chu et al)
Homocysteine is a marker for endogenous protection against oxidative attack (Lei et al, Bala et al)
Homocysteine is an amino acid that is converted into methionine within the cell; it is both a precursor and waste product and is essential for normal DNA expression and self-repair. Once methionine is used to counter oxidative stress, it is converted back to homocysteine and is ordinarily recycled again. Elevated levels of homocysteine can indicate that the cellular protective processes are being overwhelmed by oxidative attacks or that an insufficiency of one or more essential co-factors within the one-carbon cycle exists.
Good evidence indicates that either or both partners who are struggling to conceive have an insufficiency of the key metabolites. Additional studies also point to a similar insufficiency in either or both partners of couples enduring raised miscarriage rates. Progenyx provides all of the co-factors, helping to optimise your celllular health and that of your developing baby.
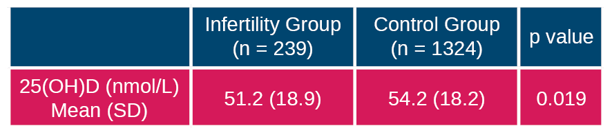
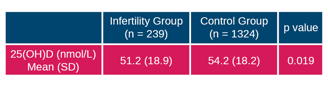
The infertility population was formed from answers to the following questions: ‘Have you or has your partner been examined for infertility?’ and ‘Have you been treated for infertility?’ Women answering ‘Yes’ to either of the questions were placed in the ‘Infertility’ group (n = 375).
The reference population included women who answered ‘No’ to both infertility questions and whose fecundability time was less than a year (n = 2051). Participants who had never tried to become pregnant (n = 754) or those with infertility problems due to their partner were excluded from the data (n = 38).
Among men, vitamin D level is the most significant indicator of seminal quality (Ciccone et al)
The relationship between the quality of eggs/sperm and pregnancy rate and the birth rate of normal healthy babies has been established in many studies of sperm parameters. It follows that as vitamin D is the most significant factor in seminal quality prospective fathers can expect to improve their chances of conceiving by ensuring they fall within the normal physiological range. Furthermore, the viability of the fertilised egg is dependent upon maintaining positive semen parameters and by doing so, it is postulated that miscarriage rate can be reduced.
25(OH)VD3 is the most significant factor in
Total number of spermatozoa
Sperm Concentration
Total number of motile spermatozoa
Total number of spermatozoa with progressive motility
Strict morphology
Interpreting the Data
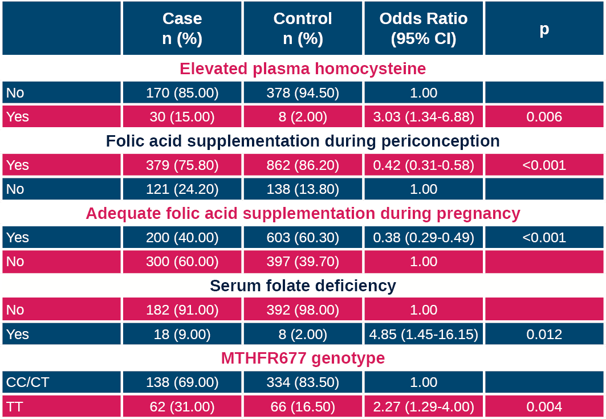
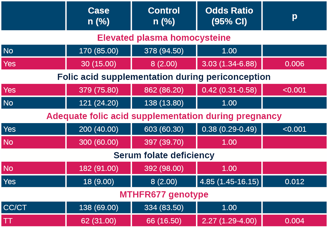
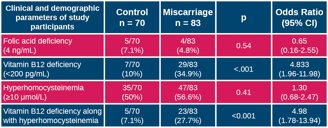
This was a retrospective study to assess underlying biochemical changes that are predictive of increased miscarriage risk. The key marker is plasma homocysteine. The authors assessed folate sufficiency prior to and during pregnancy and also tested mothers for the MTHFR677 gene that impedes normal activation of folic acid into methytetrahydrofolate. Women with this genotype should take activated folate (MTHR) - this is the form present in Progenyx.
Vitamin B12 was assessed in a handful of cases but the numbers were too low to correlate deficiency with increased miscarriage rate to statistical significance. The other vital co-factors that are required for homocysteine recycling and priming the one-carbon cycle were not assessed. The results above demonstrate that folate deficiency, the presence of MTHFR677 and elevated plasma homocysteine are closely correlated with an increased risk of miscarriage. Progenyx provides the recommended daily allowance of MTHF (activated folic acid) as well as the other co-factors involved in maintaining antioxidant capacity; its unique combination of metabolites ensures that homocysteine recycling can continue normally.
Vitamin B12 and elevated plasma homocysteine linked with early pregnancy loss (Bala et al)
A further recent study and meta-analysis demonstrated a clear link between vitamin B12 and elevated plasma homocysteine with an increased incidence of early pregnancy loss (miscarriage). Interestingly, no link was proven between folate insufficiency and miscarriage; in fact, the group of women who experienced early pregnancy loss had higher levels of plasma folate.
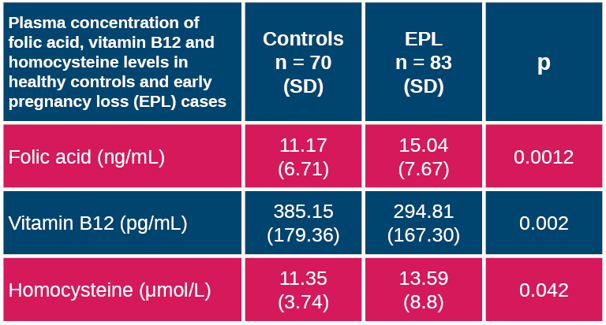
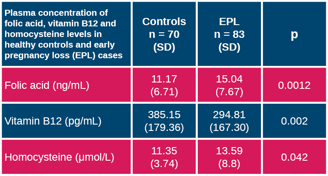
The data show the differences between the two groups of women in folic acid and homocysteine levels are statistically significant. When the test parameters are based upon the accepted reference values for both folic acid deficiency and hyperhomocysteinaemia the statistical significance disappears, perhaps suggesting that the current accepted normal levels need to be reassessed.
Women with both low vitamin B12 and hyperhomocysteinaemia were found to be at the greatest risk of miscarriage. The authors concluded that both markers were independent risk factors for miscarriage and might offer the means for screening.
Low levels of vitamin B12 and hyperhomocysteinaemia (elevated homocysteine) are risk factors for early pregnancy loss
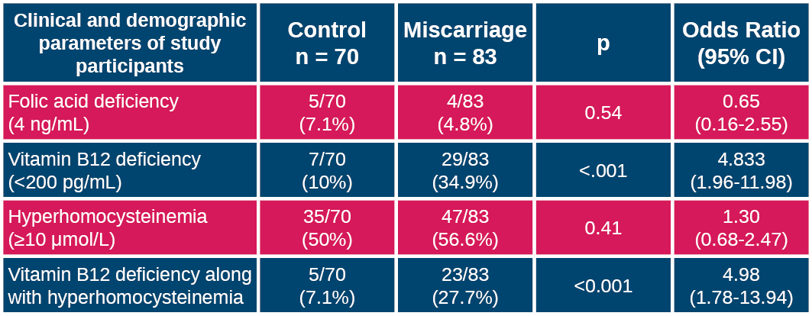
Helping women maintain normal levels of both metabolites may offer a therapeutic route to reducing the risk of early pregnancy loss.
The risk of miscarriage can be reduced if both partners have adequate vitamins B12 & D, normal plasma homocysteine and a fully functioning one-carbon cycle
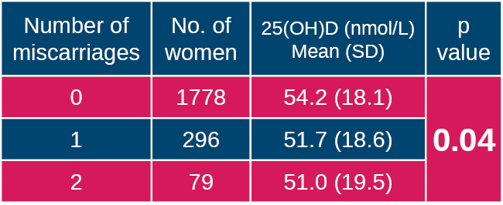
Inverse correlation between Vitamin D and miscarriage rate
As part of the study an analysis was performed to determine whether vitamin D sufficiency influences pregnancy outcome. This table assesses 3 groups of women: the first group did not miscarry (all pregnancies went to term, the second had one miscarriage and the third group experienced 2 or more miscarriages. Within the last 2 groups the women may have had a later successful pregnancy and it would have been interesting to examine whether the women who went on to have a baby had significant differences in vitamin D levels compared with those who were unsuccessful although the number of subjects may have been too few.